Cataracts
Sierra Eye Associates has three experienced cataract surgeons specializing in state-of-the-art ‘quick recovery’ cataract surgery: Gregory L. Cohen, M.D., Michael L. Stanko, M.D. and Kevin M. Gamett, M.D..
Cataracts occur as part of the normal aging process. Studies show that about 50% of all people will have some cataract formation before age 60 and close to 100% will develop them by age 70. Cataracts are the leading cause of vision loss in the world. They can severely impair your vision, but fortunately they can be treated. Today, modern surgical techniques combined with intraocular lens implantation make cataract surgery safe, fast, and effective.

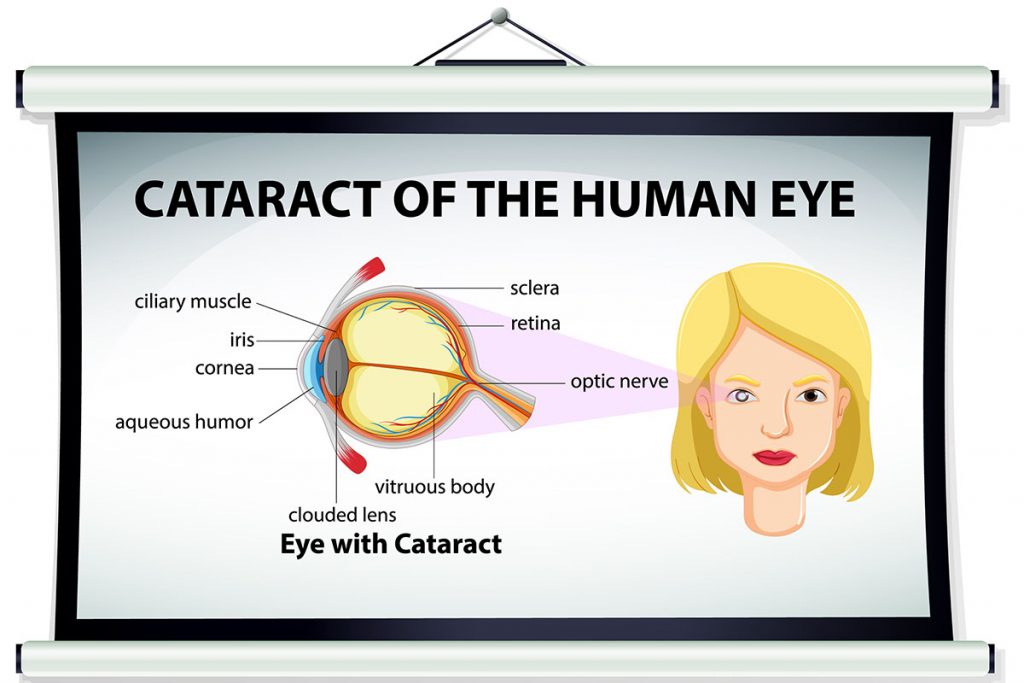
A cataract is a clouding of the normally clear lens in your eye that may cause blurred or hazy vision. As the cataract develops, the clouded lens reduces the amount of light that can enter your eye resulting in blurred or foggy vision.
It is similar to looking through a dirty window. Glare from car headlights at night, glare from sunlight, and needing more light to read can be early signs of cataract formation. Currently, there is nothing you can do to prevent the formation of cataracts.
Treatment is indicated when decreased vision affects your everyday activities or hobbies. There are several techniques to remove the clouded lens. The most common technique is phacoemulsification. A very small incision is made and a tiny high-frequency ultrasound probe is used to break up the cataract and gently suction it away. A clear membrane bag is left in your eye where an intraocular lens is placed (IOL). This lens is necessary to replace the powerful lens that turned cloudy and has been removed. The IOL has almost eliminated the need for thick cataract glasses and contact lenses that were used years ago.
The benefits to this small incision surgery is the short period of time the procedure takes and the quick recovery time. Patients are able to eat a light snack and drink immediately after surgery. Drops will be used for several weeks after surgery. Most people notice an improvement in their vision soon after surgery. You will still need glasses to read after the surgery. Your new prescription is given several weeks after the procedure.
No matter what your age, you want to enjoy an active and productive lifestyle. Improved vision will enhance your quality of life and add years to your life. If you are having difficulty with your vision, and feel cataracts may be the cause, call for an appointment at (775) 329-0286.
Glaucoma
Sierra Eye Associates provides comprehensive eye exams include glaucoma evaluations. We are proud to have two fellowship trained Glaucoma Subspecialist: Michael L. Stanko, M.D., and Kevin M. Gamett, M.D..
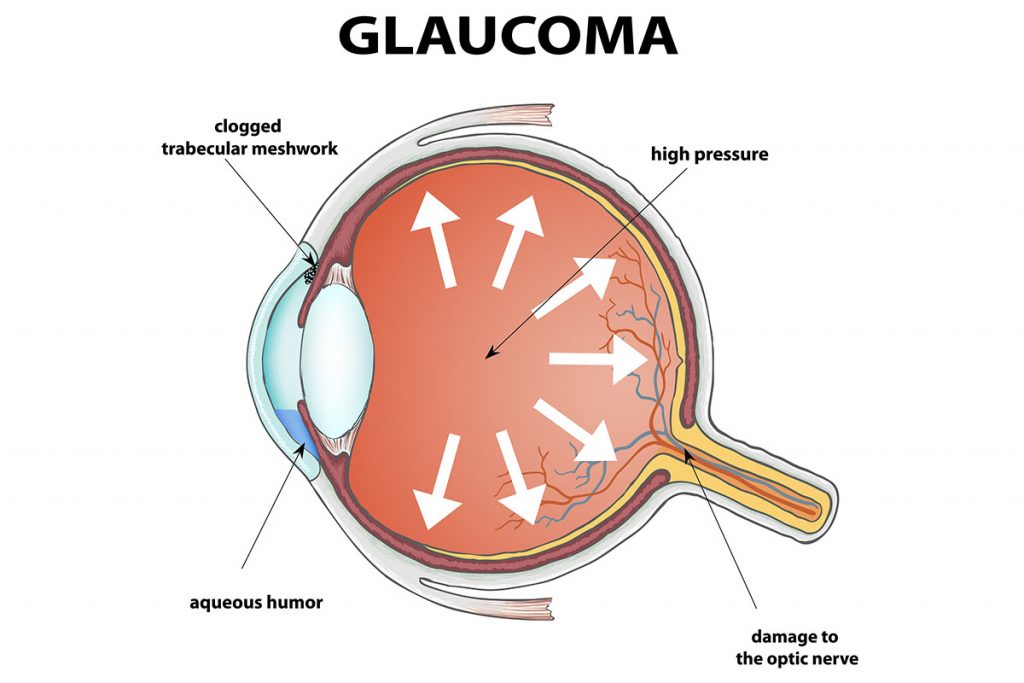
Glaucoma: Prevent the Loss with Early Diagnosis
Glaucoma is a disease of the optic nerve, and is a very common cause of blindness in older individuals, though it may begin at a young or middle age. The optic nerve is located at the back of the eye and connects the eye to the brain. When the nerve is damaged by glaucoma, there is a gradual loss of side vision, the “visual field.” Late in the disease, center vision can also be lost, which can cause blindness if the glaucoma is detected too late. Glaucoma has no symptoms. Fifty percent of those who have glaucoma are not aware of it. If glaucoma is detected early, most patients will not go blind. African-Americans may be at least four to five times more likely than white patients to develop glaucoma.
Risks of Glaucoma
The Baltimore Eye Survey examined all willing residents of a region in East Baltimore for any type of eye disease, with half of those with glaucoma not knowing they had it. This study ran through Johns Hopkins University. The rate of glaucoma was similar for men and women. In those over 40 years old, glaucoma was found overall in 5% of African-Americans and less than 1% of whites. Glaucoma becomes more common with increasing age. The rate of glaucoma above age 80 rose to nearly 3% in whites, but in African-Americans rose progressively up to over 11% above age 80, and this percentage was even higher if “glaucoma suspects” were included. A “glaucoma suspect” is a person whose optic nerve looks as if it may have glaucoma, but this cannot be proven.
Family History
Glaucoma may run in families. Ask if anyone in your family takes eyes drops on a regular basis or has a history of blindness. Close family members of a person with glaucoma should be checked for glaucoma. The highest risk is having a close blood relative who lost vision from glaucoma or who has required glaucoma surgery. This may even have a stronger relationship in African-Americans, in whom glaucoma may start at a younger age and be more aggressive. The best way to prevent vision loss is to begin regular eye exams early. It is never too early to begin regular eye exams. It may be wise to be sure you have regular exams, especially if there is a family history of glaucoma.
Glaucoma is a slowly progressive disease; patients do not usually notice any signs or symptoms of the disease until their vision is already affected. The only way for a person to know if they have glaucoma is through regular, complete eye exams, where the pupils get dilated, or enlarged temporarily with eye drops, to examine the optic nerve in detail. Wearing glasses has nothing to do with glaucoma. Patients who wear glasses may be more likely to have their glaucoma detected only because they have had their eyes examined.
Diagnosis of Glaucoma
A diagnosis of glaucoma is based on the appearance of the optic nerve. Elevated eye pressure was typically associated with glaucoma, but blood flow problems to the optic nerve may also be part of the cause. The normal eye pressure used to be considered 10-21 mm Hg. However, up to one third of all glaucoma patients may never have an eye pressure over 21 mm Hg. Eye pressure can vary quite a bit in glaucoma. While elevated eye pressure is common, patients can have high eye pressure without glaucoma, or may have damage from glaucoma with normal levels of eye pressure. Persons who have ever been told they had high eye pressure should be sure to have a complete eye exam and begin regularly scheduled exams in the future.
During the eye exam, the vision is tested, the eye pressure is measured, the internal drainage system of the eye is evaluated, and the front and back of the eye are thoroughly examined. A visual field test may also be performed. This is a standardized computer test of the side vision, or visual field. However, visual field loss may not show up early in the disease. Photographs of the optic nerve may be taken, which serve as a comparison to determine if there are changes in the future.
Types of Glaucoma
The most common type of glaucoma is chronic open-angle glaucoma. This is the type of glaucoma in which the drainage channel of the eye does not function properly and slow damage to the optic nerve occurs. Acute angle-closure glaucoma is much less common and occurs when the drainage angle suddenly closes off. This results in a sudden rise of pressure and it requires immediate attention. A person at risk for this can often be treated by a laser procedure which can prevent the sudden increase in eye pressure; this can be detected by looking for a particular shape of the drainage channel, called a “narrow angle.” Normal tension glaucoma occurs when an individual suffers optic nerve damage secondary to pressure in their eye which is within the normal range; scientists believe these patients may have a genetic predisposition to optic nerve damage. “Secondary” glaucoma usually results from a preexisting eye or medical problem, such as diabetes, trauma, blocked blood vessels, or inflammation.
Treatment of Glaucoma
While not all patients with glaucoma have high eye pressure, the eye pressure is all that is currently available to treat, and a “target” pressure level is set for each patient where the patient should not have further damage. There are different types of treatments available for lowering the eye pressure. These include eye drops, laser, or surgery. The treatment is chosen as to what is most appropriate for an individual patient; not all patients receive the same treatment. To begin treatment, patients most commonly receive eye drops, and may require only one type or several types of drops used together to reduce the eye pressure. Laser to the drainage system has also recently become accepted as a beginning treatment; this is decided with the patient on an individual basis. Surgery is used when medications and laser have failed, but there is current research to see if surgery earlier is better for the patient. The surgery, called a trabeculectomy, creates a new passage for fluid to drain out of the eye. This surgery may also be done in combination with cataract surgery when appropriate.
Glaucoma is not presently curable, but is treatable. Early diagnosis by regular eye examinations, close follow-up, and compliance with treatment are the best methods to prevent vision loss. Many medications are available for treatment, and new research is continually being done to develop new ways to treat or prevent glaucoma.
The Retina
Sierra Eye Associates are trained in recognizing and treating patients with Diabetic Retinopathy and Macular Degeneration. We have two fellowship trained vitreo-retinal specialist, Arshad Khanani M.D, M.A., and William J. Durant, M.D..
We treat all aspects of retinal diseases including diabetic retinopathy, macular degeneration, retinal detachment, macular holes, macular puckers, uveitis and pediatric retinal surgery. We offer all current treatments for vitreous diseases including intravitreal injection of Lucentis, Avastin, as well as small gauge, suture less retina surgery under local anesthesia. Our office also provides the most advanced imaging equipment including the Heidelberg Spectralis OCT.

DIABETIC RETINOPATHY
Diabetes mellitus is a condition that can have an effect on the small blood vessels of the body. One location of such small blood vessels is the retina in the eye. When the retinal blood vessels are affected, this is a condition called diabetic retinopathy.
Diabetic retinopathy development increases with the duration of the diabetes. It is unusual to see clinical signs of diabetic retinopathy prior to ten years after the onset of the disease. Diabetic retinopathy can progress with time, and has become the leading cause of legal blindness in working-aged adults. Our knowledge of treatment of diabetic retinopathy has increased over the last several years and blindness due to diabetes is becoming less frequent. In addition to treatment of the retina directly, recent studies have shown that strict blood sugar control can decrease the onset and progression of diabetic retinopathy.
Clinically, diabetic retinopathy is divided into two broad categories, non-proliferative and proliferative retinopathy.
Non-proliferative diabetic retinopathy is caused by damage to the walls of the normally present retinal blood vessels. The damage to the walls of the vessels results in leakage of blood and fluid from the small blood vessels. This leakage can result in swelling of the retina, like a sponge taking up water. If the swelling involves the macula (center of the vision) then vision is affected. Fatty material (lipid) can leak from blood vessels and can result in more permanent loss of vision. More severe damage to the retinal blood vessels can result in closure of vessels and decreased blood flow to areas of the retina. If this loss of blood flow and nutrition involves the center of the vision, significant loss of vision can result.
Proliferative diabetic retinopathy results when there is the development of abnormal (“neovascular”) blood vessels in addition to the normally present retinal blood vessels. Neovascularization results from the vascular damage resulting in lack of blood flow and nutrition to large areas of the retina. The retina becomes “starved” for oxygen, and a chemical signal is sent from damaged retina to induce the body to grow new blood vessels. This is the body’s response to provide more oxygen to those areas, but the new blood vessels are fragile and grow from the surface of the retina into the vitreous “jelly” in the center of the eye. The movement of the vitreous “jelly” and the new blood vessels can result in rupture of the fragile vessels, resulting in bleeding into the center of the eye. With time, the abnormal blood vessels can scar over, contract, and pull on the surface of the retina. This pulling can cause the retina to come away from the back of the eye (retinal detachment) and can result in permanent blindness.
Treatment of diabetic retinopathy consists of in-office laser photocoagulation and/or a surgical procedure known as vitrectomy. We also offer all current treatments for diabetic retinopathy including intravitreal injection of Avastin, steroid, as well as small gauge, suture less retina surgery under local anesthesia.
Laser photocoagulation can be used to achieve one of two goals. Laser can either cauterize blood vessels that are leaking to stop leakage or it can destroy damaged retinal tissue by creating scarring.
In non-proliferative diabetic retinopathy, vision loss can be caused by leakage from retinal blood vessels. Laser is applied to the areas of leakage to try to decrease leakage and allow the body to reabsorb leaked material. The laser is often guided by a photograph test known as fluorescein angiography. This test is performed in the office by injecting an intravenous fluorescein dye while photos are taken of the dye circulation through the retina. The risk of significant visual loss can be reduced by the use of laser in non-proliferative diabetic retinopathy.
In proliferative diabetic retinopathy, new, abnormal, blood vessel growth develops due to damaged retina that sends out chemical signals. Laser in this situation is applied to try to ablate damaged retina by creating scarring. If damaged retina is destroyed, new blood vessel growth will regress. This ablation of damaged retina requires the application of many (often more than 1000) laser burns to the peripheral retina. This may be done in one or multiple sessions, and can be done with or without anesthetic injection around the eye.
Significant visual loss can be reduced by up to 66% with the use of laser in proliferative diabetic retinopathy. There can be side effects of this more intense laser treatment, such as decreased night vision, decreased peripheral vision, and blurring of central vision.
Vitrectomy surgery is indicated when there is bleeding into the center of the eye that persists and cannot be treated with laser. At times, scar tissue formation from abnormal blood vessel growth can cause pulling on the retina and retinal detachment. Vitrectomy surgery is microscopic surgery with small instrumentation that is used to remove vitreous, blood, and certain scar tissue. Damage that results in the need for vitrectomy surgery is often advanced, and the goals of surgery are often to regain ambulating vision, but not particularly reading vision.
In summary, vision can often be maintained in diabetes. Strict blood sugar control and regular examinations for early detection are critical elements in maintaining as much vision as possible. The incidence of diabetic retinopathy goes up after 10 years of diabetes, and the frequency of examination will be determined by your eye specialist. Very close monitoring of diabetic retinopathy is necessary during pregnancy, as progression can occur. If changes of diabetic retinopathy threaten visual loss, laser photocoagulation should be considered. We often can maintain vision at a certain level, but regaining vision lost is usually not possible.
Age Related Macular Degeneration (ARMD) is a disease that affects the retina of the eye. This condition is probably hereditary in nature, but the only known association is advancing age. The retina is the inner lining of the back of the eye, like the inside of the wall of a basketball. The retina works like film in a camera. The central part of the vision, that part used for reading, is served by a portion of the retina called the macula. This is the area involved in ARMD.
The earliest sign seen in ARMD is the presence of yellow deposits below the retina, called drusen. This indicates a “tendency” toward ARMD, but typically does not cause significant loss of vision. ARMD may progress in those eyes with drusen, and therefore regular observation for the signs of ARMD is indicated.
MACULAR DEGENERATION
ARMD is clinically divided into two types. These vary in time course of vision loss, symptoms, and options for treatment.
Dry Macular Degeneration is a type where there is gradual degeneration of the cells associated with the central vision. The major symptom is usually gradual onset of increased difficulty with reading and central vision. This may occur over many years. Loss of vision can vary from mild to severe central vision loss. No specific treatment for this condition is known. There has been a lot of “talk” about the role of vitamins in ARMD, but scientific evidence is lacking. Those proponents of vitamins feel that vitamin use may help to keep the affected cells more healthy and slow down the degeneration of those cells.
Wet Macular Degeneration is a type where leakage develops under the macula. Leakage may be associated with abnormal blood vessels called Choroidal Neovascularization. If leakage is not associated with choroidal neovascularization, then typically a blister of fluid develops, and this may remain the same or slowly become larger. This can cause distortion and/or blurring of the central vision. If no choroidal neovascularization is present, then the situation is observed only, and the blister can collapse over time.
If choroidal neovascularization is present, the abnormal blood vessels are often fragile and leaky. This can result in fluid leakage or bleeding. Such changes often cause distortion, “missing areas” and blurring of the central vision. The onset of these changes can literally be over a matter of hours. We offer all current treatments for wet age related macular degeneration including intravitreal injection of Lucentis and Avastin.
Fluorescein Angiography is a test performed in the office to identify if macular degeneration is of the wet or dry type, and to determine if choroidal neovascularization is present. This involves injection of a fluorescein dye into a vein and taking pictures of the retina with a special fluorescein camera to track the flow of fluorescein through the blood vessels.
Management of patients with ARMD varies according to the type of ARMD, stage of the disease, and the treatment that may have been indicated. All patients with ARMD should check their own vision every day for any change such as decreased vision, new distortion or new missing areas. Patients are typically scheduled for regular follow-up visits to determine if there is progression, but since dry ARMD can change to wet ARMD at any time it is important that you let us know if there are new changes so we can evaluate you sooner than the scheduled follow-up visit.
ARMD is a disease that affects both eyes. One eye may have much more involvement than the other. In a patient who has had significant changes in one eye, the other eye is at somewhat more of a risk of having similar changes. Both eyes are evaluated at follow-up visits, and changes in either eye may be important.
One concern of many patients is the fear of total blindness. Fortunately, ARMD does not cause total blindness and even with total loss of central vision there is still usable peripheral vision.
Pediatrics
Sierra Eye Associates is proud to have a fellowship trained specialist in Pediatric Ophthalmology and Strabismus (eye misalignment): Pauline Hong M.D..
Our Pediatric Office is located at:
1895 Plumas Street Suite 1,
Reno, NV 89509
Why a pediatric ophthalmologist?
A pediatric ophthalmologist is a medical doctor, trained in the specialty of ophthalmology and in the subspecialty of pediatric ophthalmology and strabismus (misalignment of the eyes). Many pediatric ophthalmologists restrict their practice to children or adults with related problems and thus are particularly qualified to treat pediatric vision problems.

Ophthalmologists are medical doctors (MDs) who have had four years of medical school, one year of internship training in a hospital, and three years of residency training in ophthalmology. They are equipped to provide total eye care: they perform complete eye examinations and fit eye glasses; prescribe medications; and perform all types of laser and incisional eye surgery. Pediatric ophthalmologists have chosen to specialize in eye disorders unique to infants, children and adolescents including inherited eye diseases, amblyopia, strabismus (wandering eyes), and refractive errors (nearsightedness, farsightedness, and astigmatism). Subspecialty training in pediatric ophthalmology requires one year of fellowship.
Children’s eyes and vision are still developing after birth, so many of the diseases that affect their eyes can have a life-long impact if untreated. Pediatric ophthalmology evolved over the past 30 years in response to the exponential growth of information about children’s eye problems and advances in surgical and non-surgical techniques to address those problems. In addition, as part of their training, pediatric ophthalmologists learn how to examine a frightened or uncooperative child in a manner which is non threatening and is effective in obtaining the most information about that child’s vision. In this way a more accurate and complete diagnosis and treatment plan can be achieved.
Thus a pediatric ophthalmologist is specifically trained to diagnose and treat children with eye and vision problems. Their training and expertise uniquely qualify them to protect a child’s visual future.
Dr. Alan Johnson and Dr. Pauline Hong specialize in Pediatric Ophthalmology. Their areas of expertise include surgical correction for strabismus (wandering eyes), diagnosis and treatment for amblyopia, blocked tear ducts, congenital eye diseases, and eye examinations and glasses for children.
What is a “lazy eye”?
AmblyopiaAmblyopia, the medical term for “lazy eye” is reduced vision in an eye that can not be corrected by glasses and which has no other ocular cause (for example a scar in the eye). Many people will call an eye lazy because the lid droops or the eye wanders but these are actually distinct conditions. An amblyopic eye often appears perfectly normal, so it is often detected only through vision screening. In childhood, the connections between the eyes and the brain are just developing. The brain must learn how to put together information from the two eyes to make one picture. If the image from one eye is clear and the other blurry, or if the eyes are crossed and send two different pictures, the brain will choose to ignore the pictures being sent by one eye. When the brain consistently ignores information being sent by an eye, that eye will become weak, just as an arm, which has been in a cast, will not have equal strength to the fellow arm. Amblyopia is treatable until the age of 8 or 9 years–the age at which visual maturation is thought to be developmentally complete. Amblyopia is treated by forcing the child’s brain to use the weaker eye–this can be achieved by wearing a patch over the stronger eye, or blurring the vision in the stronger eye with glasses or eye drops. The predisposing conditions also require correction such as glasses or surgery.
What causes strabismus (eye misalignment)?
The answer is not really known. Probably it is a combination of genetic and environmental influences. Misalignment of the eyes may present as one eye appearing to look straight ahead and the other eye pointing inward, outward, upward, or downward. When a child’s eyes cross or one eye wanders, there often is loss of depth perception because the eyes are not working together. The sooner these conditions are treated, the more likely that this depth perception can be regained. The most common age for strabismus to be present is between age 2 and 4 years, although some children are born with strabismus and in others it may not be apparent until the child is older. Treatment of strabismus often requires the use of glasses, sometimes surgery, and rarely exercises. Often, amblyopia is also present which must be treated as well. Strabismus does not usually correct itself.
When should my child have a complete eye examination?
Ideally, all children should have a complete, dilated, ocular examination between the ages of 2 and 3. Unfortunately, many insurance companies will not pay for a routine examination if there is no problem found. So many parents and pediatricians rely on the vision screenings provided by local organizations. A vision screening is not a substitute for a complete examination. If there is any suspicion that the child is having difficulty seeing or has strabismus or amblyopia, the child should be examined as soon as possible. Even infants can have a complete examination so no child is too young to be examined.
Amblyopia affects 1 out of 20 children. It is the most common cause of visual loss in young people (more than eye disease and trauma combined).
Strabismus (eye misalignment) affects 1 out of 20 children. It occurs equally in boys and girls. Adults who develop strabismus usually will see double.
Glasses are prescribed for children to treat amblyopia and strabismus, and also to correct blurred vision. Glasses prescribed for blurred vision alone are simply aids to improve vision and the eyes will not be damaged if the glasses are not worn.