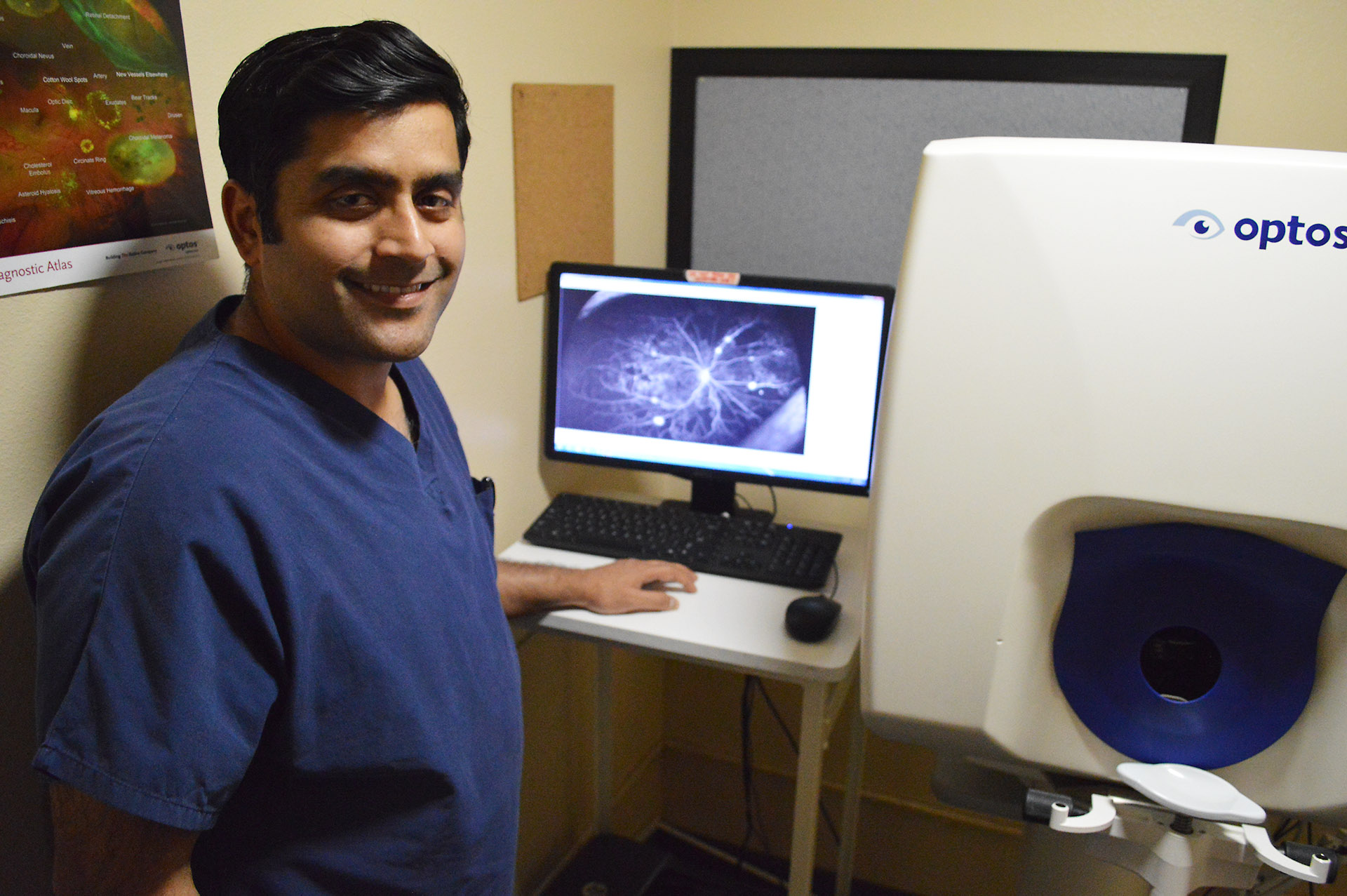
2 convenient locations with a comprehensive team of medical and surgical eye care specialists
Sierra Eye Associates is a six physician practice which has been providing the highest quality medical and surgical eye care in Reno for over 40 years.
We have on staff one fellowship-trained Glaucoma subspecialists and a Pediatrics/ Strabismus subspecialist.